| |
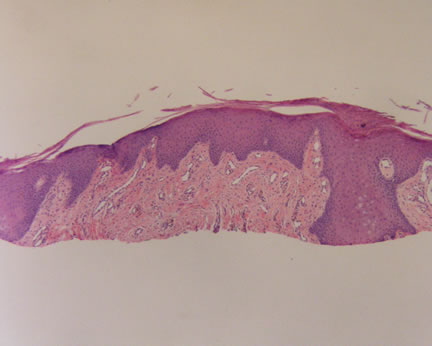 Figure 1-Low power magnification of the scar taken from the lip. The previous biopsy showed a hypertrophic actinic keratosis that extended to the shave margins. This prior original biopsy showed no atypical melanocytic proliferation Figure 1-Low power magnification of the scar taken from the lip. The previous biopsy showed a hypertrophic actinic keratosis that extended to the shave margins. This prior original biopsy showed no atypical melanocytic proliferation
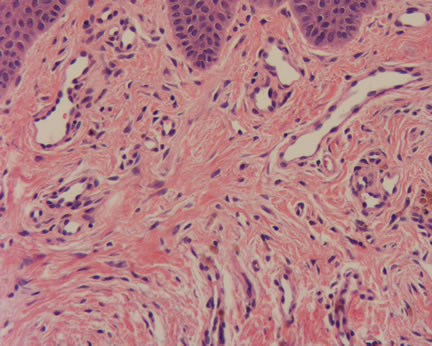
Figure 2-Higher power magnification of scar. Note the hemosiderin-laden macrophages in the center and right side of the photo.
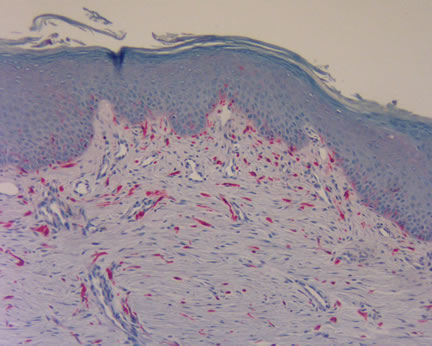 Figure 3-S100 stain decorates several of the spindle cells as well as junctional melanocytes. Figure 3-S100 stain decorates several of the spindle cells as well as junctional melanocytes.
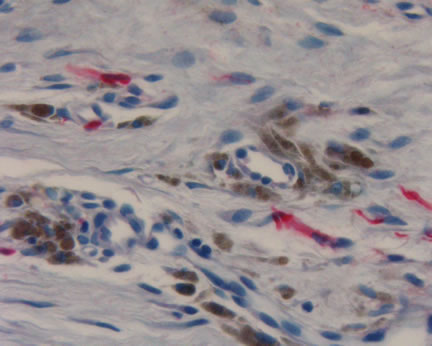 Figure 4-Higher power magnification of the S100 positive cells and the negative staining of the hemosiderin-laden macrophages. Figure 4-Higher power magnification of the S100 positive cells and the negative staining of the hemosiderin-laden macrophages.
|
|
 |
|
Issues in Dermatopathology
What is the significance of S100 positive staining spindle cells in scars?
Chorny JA, Barr RJ. Am J Dermatopathology 2002;24:309-312.
Dermatology and pathology residents are taught early on in their training, "Beware the diagnosis of a scar in sun-damaged skin!"
The warning
is rooted in the well-documented cases of desmoplastic melanoma masquerading as a clinical scar. To further complicate the issue, desmoplastic melanomas may sometimes be histologically subtle, often resembling a scar. For the unwary pathologist, the diagnosis of a scar is rendered, agreeing with the submitted clinical impression. Only later, is the diagnosis of melanoma confirmed with the recurrence of the "scar".
The S100 stain has been used to assist in the differential diagnosis of a scar versus a desmoplastic melanoma, being positive in the latter. Additional melanoma specific markers such as HMB45 and Mart-1 are usually negative in desmoplastic melanomas, and thus not helpful. However, a recent paper in the dermatopathology literature casts doubt on the specificity of S100 staining for melanomas.
In this paper, the authors compared re-excisions of cases of ten re-excised atypical nevi
and 10 re-excised melanomas. In all 20 cases, S100-positive spindle cells were identified within
the scars. The authors also compared re-excisions of non-melanocytic lesions and found a trend toward quantitatively less S100 positive cells in these scars. The authors speculate that the S100 is staining fibroblasts or less likely dermal dendritic cells.
A recent case illustrated the pitfalls of relying solely upon immunohistochemical stains for a diagnosis. Figures 1 and 2 depicted a scar, produced from a previous shave biopsy of a hyperkeratotic lesion from the lip. The original diagnosis was a hyperplastic actinic keratosis that extended to the surgical shave margins. No atypical melanocytic proliferation was present in any of the biopsies. An S100 stain highlighted numerous spindle cells in the re-excision specimen. An analysis of the spindle cells showed a bland cytology and no melanin pigmentation. Correlating the current findings with the previous biopsy, the histopathologic diagnosis was most consistent with a scar with S100 positive staining cells.
Of course, the traditional histopathologic criteria to aid in the differential diagnosis of a scar versus a desmoplastic melanoma still applies. Desmoplastic melanomas usually exhibit hyperchromatic spindle cells embedded within a myxoid background. Occasional mitotic figures may be present associated with a patchy chronic inflammatory cell infiltrate. The dermal-epidermal junction may exhibit atypical melanocytes. All of these features were lacking in our current cases.
Please comment on this case. I will post your responses anonymously.
Back to Issues in Dermatopathology
Additional References:
The Doctor's Doctor-Desmoplastic Melanomas
The Doctor's Doctor-Scars
|

